Our vision is a health care system that understands the traumatic roots of most illness and death, and is organized to help individuals and families prevent and heal from trauma as a core element of all services and care.
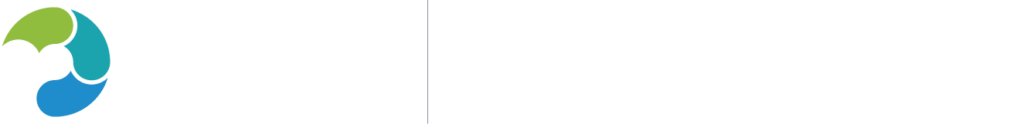
We envision the health care system moving from trauma-inducing to trauma-reducing, from treating symptoms of diseases to treating whole people:
Our Grounding Philosophy
Trauma-informed health care envisions a purposeful expansion from a biomedical focus on disease and dysfunction to a bio-psycho-social-spiritual focus on strengths and healing. We believe it requires a healthcare provider’s authentic and non-judgmental interest in patients’ life experiences. This is critically important. Patients with histories of trauma often experience healthcare and other systems as impersonal, judgmental, or harmful. For this reason, we believe that creating a safe and caring provider-patient relationship with trauma-informed care is the foundation of effective care.
This new bio-psycho-social-spiritual model of healing calls for a “triadic” approach to understanding patients and families that includes three related areas:

The TRIAD of Adversity, Distress and Strengths
- Adversity
- Signs and symptoms of Distress
- Strengths and supportive resources
Understanding this triad allows for a more “actionable,” holistic, and healing understanding of individual patients than any one area alone. It may include learning about patients’ experiences of maltreatment, discrimination, and racism as well as their sources of resilience, defined as the individual’s use of personal and community strengths as protective factors to recover from the harmful impacts of adversity.
The values that guide trauma-informed health care include: safety, trust, transparency, collaboration, empowerment, and cultural awareness, skills, and humility.
Trauma-informed Health Care: In Practice
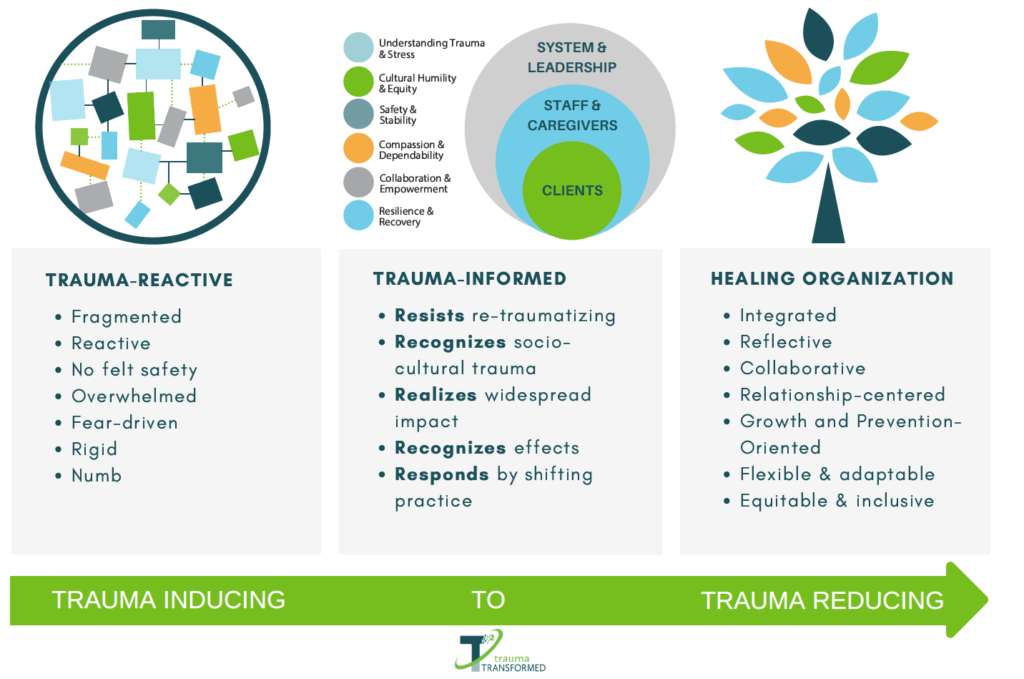
In August 2013, CTHC in partnership with the Positive Women’s Network, USA, convened a national strategy group in Washington, DC to clarify a framework for trauma-informed health care. The purpose of the strategy group was to review the evidence linking trauma to health and to provide practical guidance to clinicians, researchers, and policymakers about the core components of an effective response to recent and past trauma in the setting of primary care. The national strategy group published the new framework (pictured below) in a prominent public health peer-reviewed journal. The article can be found here. A follow-up article describing new insights into the practical delivery of trauma-informed health care can be found here.
(updated 2018)
Trauma-informed health care has five core components: a foundation grounded in trauma-informed principles and a team approach; an environment that is calm, safe, and empowering; education about the impacts of current and past trauma on health; and inquiry about and response to recent and past trauma that includes onsite or community-based resources and treatments.
Machtinger EL, Cuca YP, Khanna N, Rose CD, Kimberg LS. From treatment to healing: the promise of trauma-informed primary care. Womens Health Issues. 2015. PMID: 25965151.
For our healthcare system to live up to the needs of our families, children, and communities, it will need to be organized around understanding and responding to our patients’ adversity, distress, and strengths.