Introduction
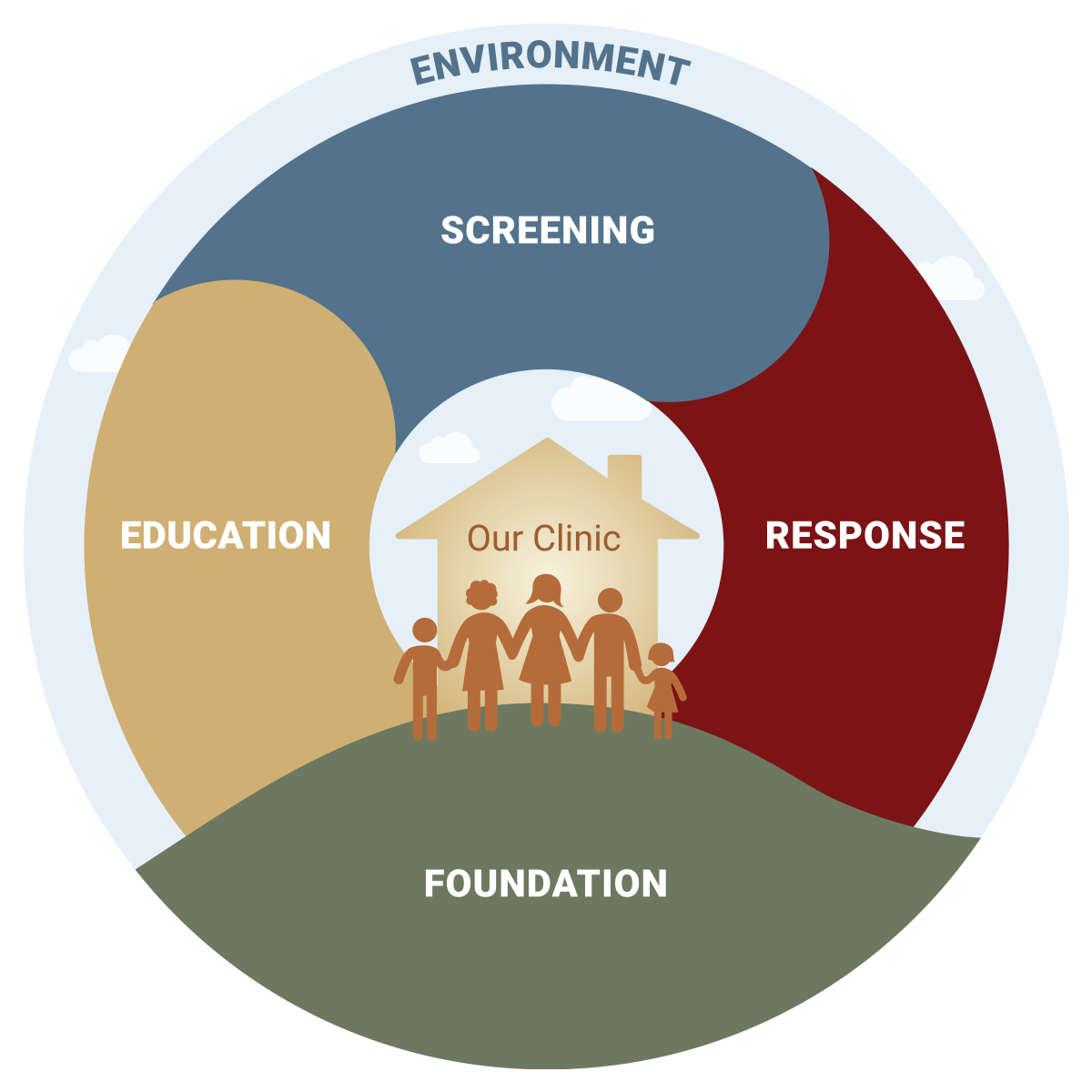
The TRIADS Implementation Approach promotes a model for trauma-informed health care that addresses adversity, distress and strengths to support healing. This implementation approach envisions ACEs screening as taking place in the context of healthcare values of equity, trauma and resilience-informed care; a safe and welcoming clinic environment; and the informed participation of patients. Several implementation studies found that ACE screening is associated with improved healthcare utilization and patient satisfaction and that patients find it useful as a bridge to the services they need.
The Approach includes 5 core elements that reflect this approach: 1) Foundation, 2) Environment, 3) Patient Education, 4) Screening and Assessment, and 5) Response. The Foundation and Environment elements establish the organizational culture necessary for effective ACEs screening and response. The other 3 elements, Patient Education, Screening and Assessment, and Response, focus on direct patient engagement and care.
Each core element has its own goals, strategies, tools, and background resources:
- Goals represent the key objectives of each element and answer the question, “What is the desired result?”
- Strategies are the actions undertaken to meet the goals and answer the question, “What do we do to reach this goal?”
- Tools provide mechanisms to carry out the strategies and answer the question “How do we do it?”
- Background Resources are key essential readings that provide contextual information, but would not be considered practical self-contained tools.
TRIADS Foundation
The TRIADS Foundation promotes trauma and resiliency-informed values; clinic champion(s); buy in from organizational leadership; interdisciplinary team-based care; community partnerships; patient/family engagement; and a commitment to health equity.
TRIADS Environment
The TRIADS Environment encourages a calm, safe and welcoming space for patients; staff receive robust training and support.
TRIADS Patient Education
TRIADS Patient Education provides all patients and families with an understanding of the connection between trauma and health, the role of protective factors, and available resources for safety and healing.
TRIADS Screening and Assessment
TRIADS Screening provides guidance on screening for adversity (immediate safety / ACEs), current distress, and strengths.
TRIADS Response
TRIADS Response to disclosures of adversity and distress should express empathy and address immediate safety. Health care providers should collaborate with patients and family on referrals to services that promote safety, connection and healing.
Foundation Tools
- Diversity, Equity, and Inclusion
A framework for leadership on Diversity, Equity, and Inclusion that focuses on the systemic environment; it uses Four W’s “Who, What, Where, and Why” to ensure that organization strategies are outcomes-oriented with secure tangible benefits for communities of color. Published by The Greenlining Institute in 2018. - Chokshi Knowledge, Attitudes, Practice
A self-administered assessment for pediatric staff on knowledge, attitude, practice related to Trauma-Informed Care. Published by S. King, K.D. Chen and B. Chokshi. in 2018. - Southern Poverty Law Center Asset Mapping toolkit
This thorough guidebook assists communities to discover the hidden assets in the community as a first step toward building positive community-based programs for children. Published by Southern Poverty Law Center (SPLC) and Alabama Youth Justice Alliance (AYJA) in 2012. - A Physician’s Practical Guide to Culturally Competent Care
A self-directed training course that enables providers to better treat the increasingly diverse U.S. population.
Environment Tools
- NCBH Trauma-Informed Organizational Assessment for Staff
Multi-page clinic assessment for trauma-informed practices developed for NCBH Change Package. Published by National Council for Behavioral Health in 2019.
Patient Education Tools
- NCTSN Trauma and Your Family
A patient handout on trauma, traumatic stress, how it can impact the family, and what families can do to cope. Published by National Child Traumatic Stress Network (NCTSN) in 2011. - Window of Tolerance graphic
A one-page infographic for patients on the window of tolerance. Published by National Institute for the Clinical Application of Behavioral Medicine in 2019. - LEAP IPV Healthy/Unhealthy Relationship checklist – English | Spanish
A 2-page (English/Spanish) self-assessment for adult patients to assess whether their relationship is healthy or unhealthy. Published by LEAP SF.
Screening Tools
- Pediatric Emotional Distress Scale (PEDS) screen for traumatic stress in children 2-10 – English | Spanish
A peer-reviewed article about the Pediatric Emotional Distress Scale (PEDS) which is used to screen for traumatic stress in children 2-10 years old; The PEDS tool (English/Spanish) is also attached. Published by Conway F. Saylor, Cynthia Cupit Swenson, Sherri Stokes Reynolds, Matthew Taylor in 1999. - Benevolent Childhood Experiences (BCEs)
A one-page scale for use with adults to identify benevolent childhood experiences (BCE). Published by Narayan, A. J., Rivera, L. M., Bernstein, R. E., Harris, W. W., & Lieberman, A. F. in 2018. - Resilience Questionnaire
A 2-page assessment for adult patients to measure resilience; this tool is used for parent education and not research. Published by Mark Rains and Kate McClinn and team at Southern Kennebec Healthy Start in 2013.
Post-screening Response Tools
- Kimberg 4C‘s
A one-page guide for providers on the Four C’s to practicing trauma-informed care (calm, contain, care, and cope) and some resources on cultural humility and healing-centered engagement. Published by Leigh Kimberg in 2019.
Additional Resources:
Race, Power, and Privilege Tools
- BSC Short Version of Racially Aware Trauma Informed Care
A four-page tool introducing four dimensions of reflecting and valuing race, identity, culture, and equitable power sharing in trauma informed practice. Published by the Baltimore Partnership for Family and Trauma-Informed Care in 2016. - Dismantling Internalized Dominance: Increasing the Capacity of Whites to Partner for Meaningful Change
A ten-page tool providing guidance for language and behavioral shifts that are core to repair of oppressive dynamics in professional settings. Published by Diane J. Goodman in 2011. - Paying Attention to White Culture and Privilege: A Missing link to Advancing Racial Equity
A journal article that discusses White culture and privilege as challenges to racial equity within organizations, and it suggests tools to address these challenges. Published by Gita Gulati-Partee and Maggie Potapchuk in 2014. - White Dominant Culture: A Worksheet
A five-page tool identifying norms of White dominant culture within organizations and providing guidance for attitudinal and behavioral shifts from such norms. Published by Partners for Collaborative Change based on White Supremacy Culture by Tema Okun and Kenneth Jones in 2019. - Racial Equity Outcome Toolkit
A thirteen-page workbook for conducting a structural race analysis, understanding an organization’s implicit and explicit assumptions, and assisting in building capacity to contribute to systemic change within an organization. Published by LaTrenda Leonard Sherrill with The Heinz Endowments in 2018. - Approaches to Power Inequity Within Organizations
A one-page handout detailing the progression of one’s organization to becoming more racially equitable. Published by AORTA in 2017. - REJI Organizational Race Equity Toolkit
A five-page worksheet for developing an organizational race equity plan. Published by JustLead Washington in 2020. - GARE Racial Equity Tool
A racial equity toolkit for guiding the development, implementation, and evaluation of policies, initiatives, and budget issues to address the impacts on racial equity. Published by the Government Alliance on Race and Equity in 2016. - King County Racial Equity Tools
A list of tools and resources designed to measure equity impact of policies or programs. Developed by King County in 2020. - Competency Modules for Equity and Privilege Awareness
Four training modules designed to increase awareness and knowledge of multicultural identities, power and privilege, oppression, and advocacy. Developed by the University of Florida Counseling & Wellness Center in 2020. - Framework for Moving from Trauma to Community Resilience (see page 29)
A one-page infographic depicting how to effectively build a framework for moving from trauma to community resilience. Published by the Prevention Institute in 2015.
Cultural Humility and Power Analysis Tools
- Community Catalyst Best Practices for White-Led Organizations to Promote Health Equity and Racial Justice in Health Advocacy
A thirteen-page toolkit to help white-led organizations ensure their health advocacy agendas, coalition work, stakeholder engagement, and communications to include, reflect, and respond to the needs of people of color. Published by Community Catalyst in 2019. - Cultural Humility: People, Principles, and Practices Video
The first segment of a thirty-minute documentary describing cultural humility and its principles, in which cultural humility as a concept is introduced and features interviews with the developers of the concept. Published by Vivian Chávez in 2012. - Cultural Humility Video
A thirty-minute documentary describing cultural humility and its principles. Published by Vivian Chávez in 2012. - Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present
A book that traces the history of medical experimentation on Black Americans in The United States since the mid-1800’s. Published by Harriet Washington in 2007.
Recruitment and Retention of Diverse Healthcare Team Members Tools
- Assessing Institutional Culture and Climate Video
A thirty-minute video providing a framework and approach to understanding and overcoming cultural and climate barriers within organizations to invest in diversity and effect equity policy change. Published by the Association of American Medical Colleges in 2013. - Toolkit for Recruiting and Hiring a More Diverse Workforce
A twenty-page toolkit on how to build diverse workforce members from posting a job to recruiting and interviewing. Published by the University Health Services at University of California, Berkeley in 2013. - Equity, Diversity and Inclusion in Recruitment, Hiring, and Retention
Toolkit with specific strategies in posting job descriptions, recruiting, and interviewing for a diverse workforce. Published by the Urban Sustainability Directors Network in 2018.
Anti-racism Tools
- RYSE Interacting Layers of Trauma and Healing, Historical Trauma
A two -page infographic contextualizing ACEs amidst historical trauma and structural racism. Published by RYSE Center in 2017. - Structural Racism Glossary
A glossary of terms related to structural racism including racial equity, white privilege, institutional racism, etc. Published by The Aspen Institute in 2018. - America Needs All of Us: A Toolkit for Talking About Bias, Race, and Change
A Toolkit for providers/leadership on Talking About Bias, Race, and Change with research-backed strategies and messages, talking points for tough questions, etc. Published by Welcoming America in 2011.
Unconscious/Implicit Bias Tools
- Strategies for Confronting Unconscious Bias
A journal article introducing types of unconscious biases and strategies for confronting them. Published by Kathleen Nalty in the Colorado Lawyer in 2016. - Harvard Implicit Association Online tests
A list of self-administered tests that assess the degree of your implicit biases towards race, age, weight, ethnicity, religion, etc.
COVID-19 Tools
- Five Cs of Leading During a Pandemic
A one-page description for leadership on 5 C’s (Clarity, Cohesion, Connect, Communicate, Courage, and Confidence) Do’s and Don’ts of leading during a pandemic. Published by Trauma Transformed in 2019. - Creating a Supportive Telemedicine Visit
A brief guide for providers with practical tips on how to create a supportive telemedicine visit including how to prepare before, during, and after the visit. Published by UCSF clinicians Brook Calton, Sarah Bellows Meister, Susannah Cornes, Jeffrey Gelfand, Marsha Blachman, Eve Cohen in 2020. - COVID Responder Self-Check
A one-page self-assessment for COVID providers and responders to assess exposure to stress. Published by MN Department of Health in 2020. - COVID Healthcare Responder Stress information
A two-page brief for COVID providers and responders on recognizing and managing stress including a list of organizational stress management policies. Published by MN Department of Health in 2020. - COVID Caregiver Toolkit for families
A toolkit for caregivers for taking care of themselves and their families during the COVID-19 pandemic; it covers supportive relationships, eating healthy, sleeping well, using movement, practicing mindfulness, supporting mental health, and spending time in nature. Published by Center for Youth Wellness in 2020. - Harvard Implicit COVID19 Online test
A self-administered test that assesses your degree of implicit bias towards coronavirus with danger and whether precautions are reasonable.